Renovascular hypertension affects up to 5% of all hypertensive patients. However, this number rises to ~30% in people with high blood pressure resistant.
This condition happens when narrowed kidney arteries trigger hormonal changes that raise blood pressure throughout the body. Understanding renovascular hypertension helps patients and doctors work together for better treatment outcomes. Additionally, early detection prevents serious complications like heart disease and kidney failure.
What is Renovascular Hypertension?
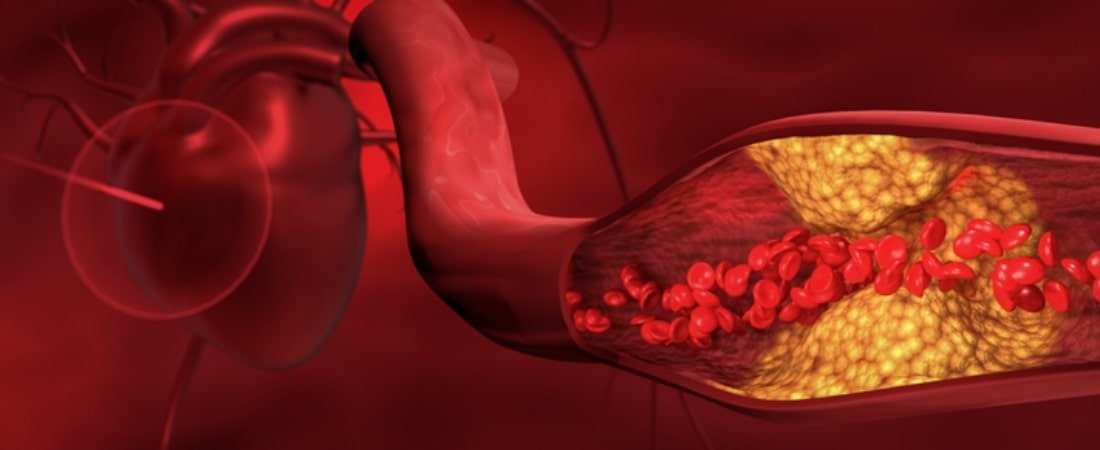
This medical condition occurs when kidney arteries become narrow or blocked. Blood flow to the kidneys drops below normal levels. Consequently, the kidneys think the body needs higher blood pressure to function properly. They release hormones that tighten blood vessels throughout the entire body.
Unlike regular high blood pressure, renovascular hypertension has a clear physical cause. Most cases of high blood pressure have no known reason. However, this kidney-related type stems from blocked or narrowed renal arteries. The kidneys control blood pressure through a complex hormone system called RAAS. Furthermore, this system normally helps maintain steady blood pressure levels.
When kidney arteries narrow, less blood reaches these vital organs. Therefore, the kidneys respond by making more hormones that raise blood pressure. These hormones affect the entire circulatory system, not just the kidneys. Moreover, the condition creates a cycle where high blood pressure damages more arteries over time.
What is renal hypertension becomes clearer when you understand this kidney-blood pressure connection. The terms “renal hypertension” and “renovascular hypertension” describe the same condition. Both refer to high blood pressure caused by kidney artery problems. Additionally, doctors may use these terms when discussing treatment options with patients.
What Are the Main Risk Factors for Renal Hypertension?
Age plays a major role in developing this condition. People under 30 or over 50 face higher risks. Young adults often have a condition called fibromuscular dysplasia. This causes abnormal cell growth in artery walls. Meanwhile, older adults typically develop plaque buildup in their kidney arteries.
Atherosclerosis ranks as the most common cause in adults over 50. This process involves fatty deposits collecting inside artery walls. Over time, these deposits harden and narrow down the blood vessels. Consequently, less blood flows through the kidneys.
Several other factors increase renal hypertension risk. Smoking damages blood vessels and speeds up plaque formation. High cholesterol levels contribute to artery blockages. Diabetes affects blood vessels throughout the body, including kidney arteries. Furthermore, a family history of heart disease raises your chances of developing this condition.
Women between ages 15 and 50 face higher risks of fibromuscular dysplasia. This condition affects the muscle fibers in artery walls. Unlike atherosclerosis, it doesn’t involve plaque buildup. Instead, abnormal tissue growth narrows the arteries. Additionally, some people inherit genetic factors that make them more likely to develop hypertensive renal disease.
Other medical conditions can also trigger this problem. Blood vessel inflammation, called vasculitis, sometimes affects kidney arteries. Tumors pressing against kidneys or their blood vessels create similar effects. Radiation therapy near the kidneys may cause scar tissue that blocks blood flow.
How Do You Recognize Renal Hypertension Symptoms?
Most people with this condition don’t notice any obvious symptoms. The kidneys work quietly, so problems often go undetected for months or years. However, doctors look for specific warning signs during routine checkups. These clues help identify when high blood pressure might be kidney related.
Sudden blood pressure changes raise red flags for healthcare providers. Previously normal readings that jump to high levels suggest possible kidney involvement. Similarly, well-controlled blood pressure that suddenly becomes hard to manage may indicate renal hypertension symptoms. Multiple blood pressure medications that don’t work properly also signal potential kidney artery problems.
Some patients experience episodes of extremely high blood pressure called hypertensive crises. These dangerous spikes require immediate medical attention. Flash pulmonary edema, where fluid suddenly fills the lungs, sometimes occurs with severe cases. Additionally, unexplained kidney function decline may point to renovascular hypertension.
During physical exams, doctors listen to unusual sounds near the kidneys. A whooshing noise, called a bruit, suggests turbulent blood flow through narrowed arteries. This finding doesn’t confirm the diagnosis but raises suspicion. Furthermore, patients with heart disease, stroke, or leg artery problems face higher risks.
Chest pain without heart artery blockages sometimes indicates widespread vascular disease. This pattern suggests that kidney arteries might also be affected. Moreover, some people notice that their blood pressure medications suddenly stop working effectively. This change often prompts doctors to investigate kidney-related causes.
What Diagnostic Tests Confirm Renovascular Hypertension?
Doctors start with a thorough physical examination and medical history review. They check blood pressure in both arms and listen to blood flow sounds. Blood tests measure kidney function and hormone levels. Urine tests check for protein or other signs of kidney failure.
Imaging studies provide the most definitive answers about kidney artery conditions. Ultrasound examines blood flow through the renal arteries using sound waves. This painless test shows if arteries are narrowed or blocked. However, it may not detect all cases of renovascular hypertension.
More detailed scans like CT angiography or MR angiography create clear pictures of kidney blood vessels. These tests use contrast dye to highlight artery blockages. They show exactly where narrowing occurs and how severe it is. Additionally, nuclear medicine scans measure how well each kidney functions separately.
Some patients need cardiac catheterization, where doctors thread a thin tube through blood vessels. This procedure allows direct measurement of pressures inside kidney arteries. Furthermore, it enables immediate treatment if significant blockages are found during the same session.
Also Read: How to Reverse Pulmonary Hypertension Naturally
What Are the Best Renal Hypertension Treatment Options?
Treatment approaches depend on the underlying cause and severity of artery narrowing. Most patients start with medications that target the kidney hormone system. ACE inhibitors and ARB medications block the hormones that raise blood pressure. These drugs often provide excellent blood pressure control for renovascular hypertension patients.
However, doctors must monitor kidney function closely when using these medications. Sometimes they can reduce kidney function temporarily while blood pressure improves. Additional medications like calcium channel blockers or diuretics may be necessary. Moreover, statin drugs help prevent further plaque buildup in arteries throughout the body.
| Treatment Type | Best For | Success Rate | Recovery Time |
|---|---|---|---|
| Medications | Most patients | 70-80% | 2-4 weeks |
| Angioplasty | Fibromuscular dysplasia | 85-95% | 1-2 weeks |
| Stenting | Atherosclerotic disease | 60-70% | 2-3 weeks |
| Surgery | Complex cases | 80-90% | 4-8 weeks |
Minimally invasive procedures work well for many renal hypertension treatment cases. Balloon angioplasty opens narrowed arteries by inflating a small balloon inside them. This procedure works especially well for fibromuscular dysplasia patients. Furthermore, doctors may place small metal tubes called stents to keep arteries open.
Surgery becomes necessary when other treatments fail or aren’t possible. Bypass surgery creates new pathways for blood to reach the kidneys. Surgeons use either synthetic tubes or blood vessels from other body parts. Additionally, some patients benefit from newer techniques like renal denervation, which reduces nerve activity in kidney arteries.
How Can You Prevent Hypertensive Renal Disease Complications?
Regular monitoring prevents serious complications from developing over time. Patients should check their blood pressure at home between doctor visits. Monthly measurements help track treatment effectiveness. Furthermore, routine blood tests monitor kidney function and medication effects.
Taking medications exactly as prescribed is crucial for success. Missing doses allows blood pressure to spike and damage organs. Setting phone reminders or using pill organizers helps maintain consistency. Additionally, patients should never stop taking medications without consulting their healthcare team first.
Lifestyle changes support medical treatments and improve overall health. Following a low-sodium diet reduces blood pressure naturally. Regular exercise strengthens the heart and improves circulation. Quitting smoking protects blood vessels from further damage. Moreover, controlling diabetes and cholesterol levels prevents additional artery blockages.
Follow-up appointments allow doctors to adjust treatments as needed. Most patients need visits every three to six months initially. These appointments check for blood pressure control and kidney function. Furthermore, they provide opportunities to discuss concerns or side effects with healthcare providers.
Frequently Asked Questions
Can renovascular hypertension be cured completely?
Treatment can control blood pressure effectively, but the underlying artery problems often remain. Procedures like angioplasty may restore normal blood flow in some cases. However, most patients need ongoing medication management. Additionally, lifestyle changes help maintain good blood pressure control long-term.
What happens if renal hypertension goes untreated?
Uncontrolled high blood pressure damages the heart, brain, kidneys, and blood vessels. Heart attacks, strokes, and kidney failure become more likely over time. Furthermore, the condition tends to worsen as more arteries develop blockages. Early treatment prevents these serious complications.
How often should blood pressure be monitored?
Patients should check blood pressure at home several times weekly. Daily monitoring may be necessary during medication adjustments. Moreover, automatic blood pressure cuffs make home monitoring easier and more accurate. Keeping a log helps doctors track patterns and treatment responses.
Are there dietary restrictions for this condition?
Most patients benefit from limiting sodium intake to less than 2,300 mg daily. The DASH diet, rich in fruits and vegetables, helps lower blood pressure naturally. Additionally, limiting alcohol and maintaining healthy weight supports treatment goals. Some medications may require avoiding certain foods like potassium-rich items.
When is surgery necessary for treatment?
Surgery becomes an option when medications and procedures don’t control blood pressure adequately. Patients with complex artery anatomy may need bypass surgery from the start. Furthermore, young patients with fibromuscular dysplasia often have excellent surgical outcomes. The decision depends on individual circumstances and overall health status.
Conclusion
Renovascular hypertension represents a treatable form of high blood pressure with identifiable causes. Early detection through proper testing leads to better treatment outcomes. Medications, procedures, and lifestyle changes can effectively control this condition. Working closely with healthcare providers ensures the best possible results.
At Koch Clinical Research, we study new renal hypertension treatment approaches to help patients achieve better blood pressure control.
Our clinical trials explore innovative therapies and procedures for this challenging condition. For more information, you can contact our research team to learn about current studies and whether you might qualify to participate.






