Because the liver plays a central role in filtering blood and supporting digestion, any problem with this system can affect the whole body.
In this article, we will explore what portal hypertension is, the main causes, common symptoms, and available treatment options. Our goal is to provide clear information so patients and families can better understand the condition and know when to seek medical help.
What is Portal Hypertension?
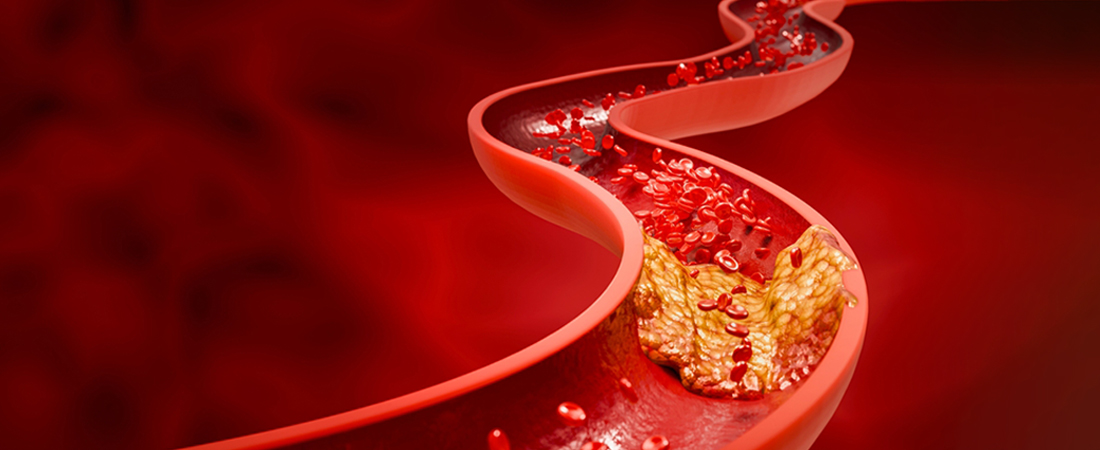
Portal hypertension means abnormally high blood pressure in the portal vein system. The portal vein is responsible for carrying nutrient-rich blood from the stomach, intestines, and spleen into the liver. Once the blood reaches the liver, harmful substances are filtered out, and nutrients are processed.
When this blood flow becomes blocked or slowed, the pressure inside the portal vein rises. This is known as portal vein hypertension. Over time, this increased pressure can cause blood to bypass the liver and flow through smaller veins in other areas, such as the esophagus or stomach. These smaller veins are not built to handle high pressure, so they can swell and sometimes burst, leading to dangerous bleeding.
In simple terms, portal hypertension is not a disease on its own but a complication of other liver problems. It usually develops because of scarring in the liver, which prevents normal blood flow.
What Causes Portal Hypertension?
Several medical conditions can cause portal hypertension. The most common cause is cirrhosis, a condition where healthy liver tissue is replaced with scar tissue. Cirrhosis may result from long-term viral hepatitis, alcohol-related liver disease, or nonalcoholic fatty liver disease. Scar tissue makes the liver stiff and blocks blood flow, raising the pressure in the portal vein.
Another cause is blood clots within the portal vein. A clot prevents blood from flowing smoothly, increasing the pressure.
In certain parts of the world, schistosomiasis, a parasitic infection, can also lead to portal hypertension. The parasites cause inflammation and scarring in the liver, which affects blood flow.
Rarely, structural abnormalities in the liver or veins can create the same problem.
It is important to note that not everyone with these risk factors will develop portal hypertension. The severity depends on how much of the liver is affected and how well the remaining tissue continues to function.
What are the 5 Main Symptoms of Portal Hypertension?
Portal hypertension often develops quietly in the early stages. Many people do not notice problems until complications appear. The five most common symptoms and signs include:
- Enlarged veins (varices): These swollen veins form in the stomach or esophagus. They may rupture and bleed, which can cause vomiting blood or black stools.
- Ascites (fluid buildup): A swollen abdomen caused by fluid collecting inside. This may feel uncomfortable and make it difficult to breathe or move.
- Enlarged spleen (splenomegaly): A swollen spleen can cause pain or a sense of fullness in the upper left side of the abdomen. It may also lower blood cell counts.
- Bleeding problems: Because the liver plays a role in clotting, portal hypertension may increase the risk of frequent nosebleeds, bruising, or serious internal bleeding.
- Confusion or forgetfulness (hepatic encephalopathy): When the liver cannot clear toxins from the blood, they may affect the brain, leading to confusion, poor memory, or changes in behavior.
Not every patient experience all of these symptoms. Some may only have mild signs, while others may develop sudden complications.
How is Portal Hypertension Diagnosed?
Doctors use a combination of medical history, physical examination, and tests to diagnose portal hypertension.
- Ultrasound: This imaging test checks blood flow through the portal vein and can show enlarged veins or fluid in the abdomen.
- Endoscopy: A thin camera is passed through the throat to look for swollen veins in the esophagus or stomach.
- CT or MRI scans: These provide detailed images of the liver and blood vessels.
- Blood tests: These help measure liver function, blood clotting, and overall organ health.
Sometimes, a doctor may recommend more specialized tests, but not everyone will need invasive procedures. Diagnosis focuses on understanding the severity of the condition and ruling out other possible causes of symptoms.
What are the Portal Hypertension Treatment Options?
Treatment for portal hypertension depends on its cause and severity. The main goals are to lower pressure in the portal vein, prevent complications, and treat underlying liver disease.
- Lifestyle and medical care: Doctors often recommend limiting salt intake, avoiding alcohol, and eating a balanced diet to support liver health. Regular follow-up visits are key.
- Medications: Non-selective beta-blockers, such as propranolol, reduce blood pressure in the veins and lower the risk of bleeding from enlarged veins.
- Endoscopic procedures: If varices are found, doctors may use band ligation, where tiny rubber bands are placed around the veins to stop them from bleeding.
- Shunt procedures (TIPS): A transjugular intrahepatic portosystemic shunt, or TIPS, is a procedure where doctors create a pathway inside the liver to reduce pressure. This helps blood flow more easily.
- Liver transplant: For severe cases where liver damage is extensive, a transplant may be the only long-term solution.
While treatment may not completely cure portal hypertension, it can control symptoms and reduce serious risks.
Can Portal Hypertension Be Reversed?
Whether portal hypertension can be reversed depends on the cause. If it is due to a temporary clot or a treatable infection, blood flow may improve once the problem is corrected. However, in most cases linked to cirrhosis, the damage is permanent.
That said, treatments can make a big difference. By controlling pressure and preventing complications, patients can live longer and more comfortably. Early diagnosis and medical care improve outcomes significantly.
Also Read: How to Reverse Pulmonary Hypertension Naturally
Living with Portal Hypertension: What Should Patients Know?
Living with portal hypertension requires ongoing care and attention. Patients should:
- Keep regular appointments with their healthcare team.
- Take prescribed medications as directed.
- Watch for signs of internal bleeding, such as vomiting blood or black stools, and seek urgent care if they occur.
- Follow dietary advice, including reduced salt intake, to manage fluid buildup.
It is important for patients to remember that not every person with portal hypertension will face the same challenges. Some may experience mild symptoms, while others may need advanced treatments. Staying informed and proactive helps reduce risks.
Symptoms vs. Possible Complications
| Portal Hypertension Symptom | Possible Complication |
|---|---|
| Varices (enlarged veins) | Bleeding, anemia |
| Ascites (fluid buildup) | Infection, discomfort |
| Enlarged spleen | Low blood counts |
| Confusion (encephalopathy) | Memory and focus issues |
| Fatigue | Reduced quality of life |
FAQs
Is portal hypertension always linked to cirrhosis?
Not always. While cirrhosis is the leading cause, portal hypertension may also result from blood clots or infections like schistosomiasis.
What are early warning signs of portal hypertension?
Early signs may include a swollen spleen, fluid buildup in the abdomen, or enlarged veins in the esophagus. Sometimes it is only detected during routine tests.
Can lifestyle changes slow progression?
Yes. Avoiding alcohol, limiting salt, and following medical advice can help manage symptoms and reduce risks.
When should I see a doctor?
Anyone with liver disease or unexplained abdominal swelling, bleeding, or confusion should seek medical evaluation right away.
Conclusion
Portal hypertension is a serious condition, but it can be managed with proper medical care and timely lifestyle changes. Understanding its causes, symptoms, and treatment options allows patients to take action before complications arise. Not everyone with portal hypertension will face the same challenges, and many people can continue to live well when they stay connected with their healthcare team.
At Koch Clinical Research, we are dedicated to supporting patients through education and clinical studies.
For individuals interested in exploring new treatment options, our ongoing hypertension clinical trials may provide access to research-based care. Taking early steps today can help improve tomorrow’s outcomes.






